- 1 Understanding Perimenopause
- 2 How does conventional HRT differ from a natural approach to perimenopause?
- 3 What are the best natural treatments for perimenopause?
- 4 What should I not do during perimenopause?
- 5 What to avoid to reduce perimenopause symptoms
- 6 Medicinal cannabis as a natural treatment option
- 7 When to seek professional help
- 8 Conclusion
Perimenopause is the natural and gradual transitional period which occurs before menopause, clinically recognised by changing menstrual patterns and fluctuating hormone levels.
Some women are fortunate to sail through this time, but sadly, others may be worried by a confusing set of associated symptoms such as brain fog, anxiety, hot flushes, night sweats, mood swings, joint pain, sleep disturbances, increased abdominal fat, hair loss, vaginal dryness, and reduced libido.
Perimenopause usually begins in a woman’s mid to late 40s, typically spanning several years, sometimes for over a decade, until menopause is considered to have occurred, which is when she has experienced a full 12 months without any periods or bleeding at all.
Until recently a taboo subject, but thanks to women such as Davina McCall, menopause has become an acceptable subject, and finally, more scientific research into effective natural treatments is being undertaken. While hormone replacement therapy (HRT) remains the standard medically prescribed treatment, growing numbers of women are seeking more natural remedies, including medicinal cannabis, for symptom relief.
This article reviews clinically studied natural options, with insights into their safety and efficacy, and will hopefully reassure you that the hormonal rollercoaster you may be experiencing can be tamed, and some hormonal harmony re-established.
Lyphe Clinic is the UK’s leading medical cannabis clinic and we provide safe, legal and accessible treatment for many chronic and complex medical conditions. The medicinal cannabis aids we provide for perimenopause, as alternatives or adjuncts to HRT, are sourced from highly reputable and professional producers, whose plants are grown in immaculate and heavily scientifically regulated conditions.
There are various forms of taking medicinal cannabis, such as inhalation, oral and topical products, which can be prescribed to help you, each specific for whatever menopausal symptoms are a concern.
Understanding Perimenopause
As you will see from the diagram below, there are essentially four stages in the menopause timeline.
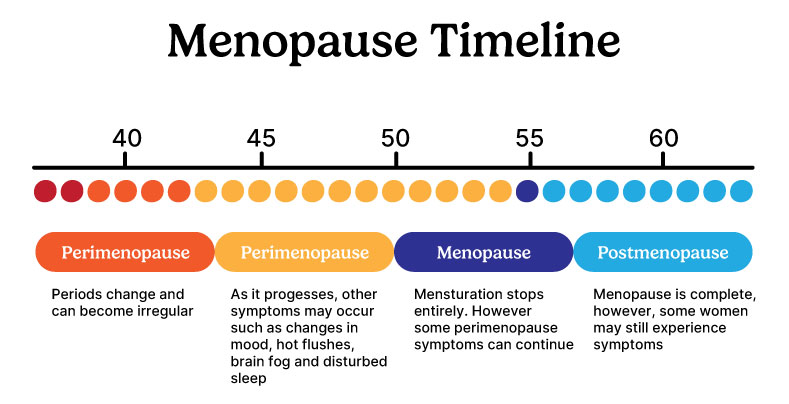
Perimenopause begins with subtle hormonal fluctuations-especially in oestrogen and progesterone-that cause menstrual irregularity, such as cycle length lasting longer than 7 days, and no longer with a regular 28-day interval.
Various symptoms for example, memory fog, joint pain, anxiety, hot flushes, mood swings and loss of libido can occur, causing distress and embarrassment.
Whilst perimenopause is a multi-year hormonal transition, with variable symptoms, the menopause, by contrast, is a specific clinical milestone – 12 consecutive months without menstruation, marking the end of a woman’s reproductive capability and a new hormonal baseline.
Understanding this distinction can help you plan better symptom management during this midlife period.
Key Differences Between Perimenopause vs. Menopause
|
Feature |
Perimenopause |
Menopause |
|
Menstruation |
Irregular periods, possibly heavier/lighter; ovulation still possible |
No periods for 12 months; ovulation ends |
|
Hormones |
Fluctuating (bounces up and down) |
Consistently low oestrogen/progesterone |
|
Symptoms |
Often more intense—hot flushes, mood swings, sleep issues, vaginal / libido issues |
Can persist, but stabilise; bone density and heart risk become more prominent |
|
Fertility |
Declining but still possible |
Absent with no possibility of natural pregnancy |
How does conventional HRT differ from a natural approach to perimenopause?
Traditional, or medically prescribed Hormone Replacement Therapy (HRT) effectively replaces hormones to relieve menopausal symptoms and maintain bone density but it comes with side effects and some rare serious risks (cancer, blood clots, cardiovascular). Natural approaches, especially bioidentical HRT and transdermal patches, may be gentler and customisable but they still carry the same fundamental risks, and there are fewer clinical studies to validate their safety or efficacy. Due to the potential side effects and risks, some women are now preferring to look for alternative, natural remedies.
HRT replaces the hormones – typically oestrogen, sometimes combined with progestogen if the woman still has a uterus-that naturally decline during perimenopause and menopause.
These hormones are administered via oral tablets, transdermal patches, gels, or injections. Oestrogen alleviates symptoms like hot flushes, night sweats, vaginal dryness, mood instability, and helps prevents bone loss; the progestogen is added if the uterus is intact to reduce uterine cancer risk.
NHS England and NICE (National Institute for Health and Care Excellence) recognise that some women prefer to use herbal and complementary remedies, but these aren’t endorsed or routinely prescribed due to limited evidence, unknown safety, variable quality, and potential interactions with prescribed medication.
Generally, symptoms during perimenopause are not static and will fluctuate and change over the period of time between perimenopause to post menopause. Symptomatic care that integrates both natural and conventional therapies often provides the best outcomes.
What are the best natural treatments for perimenopause?
Whilst some of the common symptoms of perimenopause are daunting and debilitating, it is reassuring to know that there are several herbal and nutritional supplements, alongside lifestyle considerations and stress reduction techniques, that may help you manage these perimenopausal symptoms.
Herbal, Vitamin & Mineral Supplements
- Black Cohosh: (capsules, tincture or a tea) Some randomised controlled studies have found this helpful for easing hot flushes, night sweats, and mood swings. It helps control the heat mechanism of the body and is a calming herb, helping anxiety.
- Dong Quai: (Capsule, liquid or powder) a herb also known as ‘female ginseng’, used to support female reproductive health. In both peri & post menopause, it helps with hot flushes, mood swings. fatigue, vaginal dryness and low libido.
- Vitamin D: (Capsule / tablet) Helps with bone health and mood regulation. Best to take between 1000iu – 2000 iu
- Calcium : Supports bone density, especially as oestrogen levels drop. The best type to buy is calcium citrate as this is the most absorbable and gentle on the stomach (200mg – 500mg tablets)
- Magnesium: Can reduce anxiety, improve sleep, and alleviate muscle cramps. Best to buy the a tablet form – magnesium glycinate, as it is the most absorbable & gentle on the stomach
- Omega-3 Fatty Acids: (capsules / liquid) help support heart health, reduced anxiety, reduced brain fog and reduced joint pain.
- Evening Primrose Oil: May help balance hormones and reduce breast tenderness.
Nutritional Supplements
- Flaxseed: is rich in phytoestrogens (plant compounds which mimic our body’s natural oestrogen); can help with hormonal balance.
- Ashwagandha: (Capsules, powder, tincture) Also known as ‘Indian Ginseng’, is an adaptogen (a substance that can help balance the body when it is out of kilter) that can help with stress, fatigue, thyroid support and mood swings.
- Maca Root: (Powder, capsule or tincture) A plant-based supplement that may help balance hormones and improve energy levels. It has been especially linked with enhancing libido, which often suffers during the perimenopausal hormone turmoil.
- Probiotics: (Capsules, powder, liquid – yoghurt, kefir, kimchi, sauerkraut, kombucha, miso, tempeh) Support gut health, which can impact mood and hormone balance. You will be forgiven for being confused by the term ‘Probiotic’, which is often confused with both ‘Prebiotic’ and ‘Postbiotic’. A prebiotic is the food we eat to gain the live bacteria, which are the actual ‘probiotics’, whereas postbiotics are the substances created by the growing bacteria, for example anti-inflammatory compounds in the gut. A good analogy to understand the differences is that of the Garden: Probiotics are the garden seeds we plant; Prebiotics are the fertilisers (fibre-rich foods in our diet that help the seeds grow); with Postbiotics being the harvest (fruit or veg) from the garden.
- Phytoestrogens*: (plant compounds which mimic our body’s natural oestrogen); found in soya beans / soy products; red clover; legumes (beans, peas, lentils); oats, barley, rye, brown rice; seeds and nuts, such as sesame, sunflower, pumpkin, walnuts, almonds; some fruit (dried apricots, dates, prunes) and leafy green vegetables.
*Phytoestrogens are NOT oestrogen, but they act as weak oestrogens in your body. Any woman who has suffered from any hormone-sensitive cancers should consult their healthcare professional if considering taking any of these supplements.
Lifestyle Considerations
- Yoga and Tai Chi: both as exercise and mindful meditative practices, yoga and tai chi may improve mood, sleep, and quality of life. Good interactive activities with other people.
- Diet and Exercise: Weight management, regular exercise, and a balanced diet can mitigate symptoms and improve overall health.
- Stress Reduction Techniques
- Medicinal cannabis: scientific clinical evidence has demonstrated a reduction in sleep disturbances, mood swings, hot flushes, and reduced bone loss due to oestrogen deficiency. At Lyphe, we provide an excellent supportive service, prescribing the best form and strength to aid your symptoms.
- Cognitive Behavioural Therapy (CBT): there is a wealth of good evidence which supports CBT for helping manage hot flushes, anxiety and depression, and general mood fluctuations.
What should I not do during perimenopause?
- Whilst it is good to know what can help you during this challenging time, being aware of what not to do during perimenopause can help you navigate this transition more smoothly. Here’s a list of things to avoid (or approach with caution):
- Don’t ignore your symptoms: Fatigue, mood swings, irregular periods, brain fog, hot flushes aren’t just “in your head’ but are acknowledged, genuine symptoms of perimenopause. Dismissing them could delay you experiencing helpful interventions.
If symptoms are affecting your quality of life, do talk to your healthcare professional. There are both conventional and natural therapy options (lifestyle changes, therapies, medications) to help you.
- Cut down on alcohol or caffeine: Both can exacerbate hot flushes, night sweats, sleep problems, and anxiety.Moderation helps—keep an eye on how your body responds.
- Don’t skip regular health checks: Perimenopause may increase your risk for osteoporosis (weakening bones), high cholesterol, and cardiovascular disease.
- This is the time to stay on top of screenings (e.g., blood pressure, hormone levels, thyroid function, cholesterol, mammograms, bone density).
Don’t neglect strength training and weight-bearing exercise
Muscle loss and bone thinning can sometimes accelerate during perimenopause.
Avoiding exercise may increase your risk of fractures and weight gain. Weight training is one of the finest exercise regimes you can start, as it helps build muscle and keeps your bones strong for later life.
- Do check before purchasing lots of supplements: Herbal remedies (e.g., black cohosh, dong quai) and over-the-counter menopause supplements may interact with current medications or have side effects. Check with your doctor before starting anything new.
- Don’t isolate yourself emotionally: Mood changes and anxiety are common, but suffering silently can make them worse. Try to avoid withdrawing into yourself, but reach out to friends, family, support groups, or mental health professionals.
- Don’t follow extreme diets: Crash dieting can mess with metabolism, energy levels, and mood. Instead, focus on balanced, nutrient-rich meals to support hormonal shifts.
- Don’t assume it’s all perimenopause: New or severe symptoms, for example, very heavy bleeding, severe depression, chest pain, should not be dismissed as “just hormones.” They could indicate something else that needs medical attention.
What to avoid to reduce perimenopause symptoms
If possible, try to avoid stressful situations, since chronic stress will spike cortisol in your body, which then exacerbates problems such as memory fog, insomnia, mood swings and can unfortunately, lead to increasing abdominal fat.
You will also find that too much alcohol, sugar, refined carbohydrates, and ultra-processed food will also worsen hot flushes, brain fog and increase your weight.
Establishing a sensible bedtime routine, with no screen time at least an hour prior to bed, will help avoid fatigue and increased hormonal imbalance. To have a reasonable night’s sleep, try to go to bed with a positive attitude, and employ some ‘stress buffers’, which will help overcome the dread of a wakeful night. Five to ten minutes of mindfulness as you wind down, and gentle breathing exercises as you lie in bed, can calm cortisol levels, helping you relax, and ease symptoms.
Do ensure you stay well hydrated: one to two litres of water, herbal teas and the occasional tea or coffee are good. Excessive caffeine and alcohol will likely trigger night sweats and restless legs.
Medicinal cannabis as a natural treatment option
Emerging clinical evidence from randomised controlled trials, suggests that medicinal cannabis may help alleviate some perimenopausal symptoms, particularly those related to anxiety, mood, sleep, and pain.
While clinical research on medicinal cannabis for perimenopausal anxiety is still emerging, several studies and ongoing trials have provided insights into its full potential benefits and limitations.
Our body’s natural endocannabinoid system (ECS) plays a natural role in regulating mood, pain perception, sleep, and temperature control. At Lyphe, our medicinal cannabis products, available via prescription, contain pure phyto-cannabinoids such as THC (tetrahydrocannabinol) and CBD (cannabidiol), which interact with our body’s natural ECS receptors (CB1 and CB2), thereby helping to modulate these distressing symptoms.
A 2020 cross-sectional study published in Menopause found that over 27% of midlife women reported using cannabis for menopause-related symptoms, most commonly for sleep and mood disturbances.
It is essential for women considering natural remedies to consult with healthcare professionals experienced in menopause management. In line with our high standards of care and clinical excellence, prescribing of medicinal cannabis through Lyphe Clinic, will be approached meticulously, considering each woman’s individual medical history, current health status and concerns.
A personalised and specific treatment plan will be drawn up by one of the Lyphe Clinic’s doctors, and a suitable prescription will be written for you. Follow up appointments will ensure you are happy with your prescription and any changes will be undertaken to give you the best possible outcome with regard to symptom relief.
When to seek professional help
If symptoms interfere with work, relationships, or well-being, it may be time to explore treatment for perimenopause UK from a specialist.
At Lyphe Clinic, our doctors create tailored medical cannabis treatment plans that combine clinical expertise with natural approaches to symptom relief.
Conclusion
Natural remedies, including medicinal cannabis, show promise for managing perimenopausal symptoms, though, as with all medication, further research is needed. Women should ensure there has been shared decision-making with their clinicians, allowing them to navigate all options safely and effectively.
Lyphe Clinic offers compassionate, expert-led care—book your consultation and explore the Lyphe blog for more resources.
Penelope Commerford RN NIP
References:
- Babson KA, Sottile J, Morabito D. Cannabis, cannabinoids, and sleep: a review of the literature. Curr Psychiatry Rep. 2017;19(4):23.
- Newson L. Menopause and sleep: an update. Climacteric. 2020;23(4):329–336.
- Taylor M, et al. Phytoestrogens and menopausal health: A systematic review. Maturitas. 2011;68(4):331–339.
- Webber K, et al. Cannabis use in women during the menopause transition: a cross-sectional survey. Menopause. 2020;27(10):1150–1156.
- The British Menopause Society.
- NICE / NHS (England) guidelines for menopause care.
If you would like to read more about women’s health, you may enjoy the following blog articles.
Endometriosis Treatments, Symptoms & Natural Relief
Medical Cannabis for Women’s Health

Book an online appointment
Lyphe is your patient-first path to wellness, so book an appointment with one of our medical cannabis expert Doctors and get the relief you need.
Disclaimer
The content provided on this blog is intended for educational purposes only and should not be construed as medical advice. We strongly advise readers to seek guidance from a qualified healthcare professional regarding any medical concerns.
To reflect its medicinal nature rather than recreational use, we prefer the term ‘medical cannabis’ over terms such as ‘marijuana’, “grass”. or ‘dope’ which may carry negative connotations.
The opinions expressed in the blog belong to the respective authors, who are not medical professionals, and may not necessarily align with those of Lyphe Clinic. Lyphe Clinic does not endorse any specific products or services mentioned, except those provided through Lyphe Clinic.
Readers should be aware that the legality of medical cannabis varies by location, and this disclaimer may be subject to periodic updates.
Related Insights
Whilst you’re here you might also like to read…